Ghana Priorities: Malaria
Technical Report
The Problem
According to the Global Burden of Disease (GBD), malaria represents the largest cause of death and morbidity in the country as measured by disability-adjusted life years (DALYs) (IHME, 2019). In 2017, the disease was responsible for around 19,000 deaths, almost as much as the combined death toll from HIV/AIDs and tuberculosis (IHME, 2019).
The GBD estimates 5.9m incident cases per year or equivalent to one case for every five people (IHME, 2019). Malaria puts a significant strain on the health system with a third of all outpatient department (OPD) visits being for suspected cases of malaria (Ghana Health Service, 2019).
Malaria also takes a large toll on the economy. On average, 13.5 percent of individuals in the prime working-age range of 15-49 contract malaria annually (IHME, 2019). If each case of malaria takes five days to fully recover, a simple estimation suggests 2 percent of all potential working days are lost to malaria. A survey of 62 firms in the Greater Accra, Ashanti and Western Regions showed 40 percent of all lost work-days were due to malaria (Nonvingon et al., 2016). An older study indicated that a 1 percent increase in malaria morbidity reduced economic growth in the country by 0.41 percent per annum (Asante and Asenso-Okyere, 2003). UNICEF (2007) estimated the annual economic burden of malaria be 1.0% to 2.0% of gross domestic product (GDP) in Ghana. Sachs and Malaney (2002) opine that malaria-endemic regions tend to have an average growth per capita GDP of 0.4% per year compared to a 2.3% average per capita GDP per year for non-endemic regions.
Intervention 1: Distribute and Sustain 90% Coverage of LLIN
Overview
Despite substantial successes achieved in malaria prevention in Ghana, the country is yet to achieve the NSP goal of reducing malaria burden by 75% by 2020. Since 2002, the government of Ghana has prioritized ensuring access to and increasing the use of LLINs to reduce malaria-associated morbidity and mortality. One of the key objectives of the National Malaria Control Programme (NMCP) is to reach and sustain universal LLIN coverage, which is defined as one LLIN for every two persons.
The bed nets distribution intervention targets 90 percent of households in Ghana. Given a baseline population of 31 million, 3 million bed nets distributed and 56 percent of the population effectively covered by bed nets in 2018, it is envisaged that the intervention will increase the number of bed nets distributed via continuous distribution by 2m to 2.5m per year, eventually reaching the 90 percent target in 2021 and sustaining this level indefinitely.
Implementation Considerations
To achieve this target LLIN coverage would require a 70% increase in LLIN distribution over current levels. This would require extra funding for the National Malaria Control Program (NMCP) of GH¢ 45m initially rising to GH¢ 73m by 2030 (in 2018 GH¢). This would represent a non-trivial expansion of current program activities by the NMCP.
Costs and Benefits
Costs
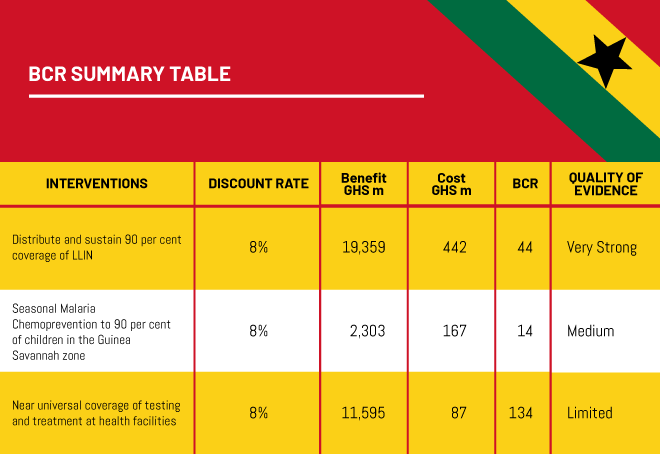
Costs estimated to represent the full procurement and distribution costs of bed nets, based on evidence of large-scale LLIN distribution in Ghana. Distributing 2 to 2.5 million extra bed nets would cost GH¢ 45m initially and rises to GH¢ 73m by 2030. The total net present cost of this intervention between 2018 and 2030 is GH¢ 442m at an 8% discount rate.
Benefits
Epidemiological modeling indicates that scaling up mass distribution of LLINs and rapid diagnostic testing have very large absolute impacts on burden and deaths avoided. Increasing coverage of LLINs from 56 percent to 90 percent will avoid 12.9m cases of uncomplicated malaria, 696,000 cases of severe malaria and 40,390 deaths between 2018 and 2030. The study estimates avoided morbidity benefits of GH¢ 9 million, mortality avoided benefits of GH¢ 139 million in 2018, with benefits expected to increase to GH¢ 230 million and GH¢ 4,803 million respectively in 2030.
Intervention 2: Seasonal Malaria Chemoprevention to 90% of Children in the Guinea Savannah Zone
Overview
Despite the many interventions in place, the burden of malaria remains high and new preventive and control measures are of necessity to augment the existing measures. Seasonal malaria chemoprevention (SMC), formerly known as an intermittent preventive treatment in children (IPTc), has been identified as a potentially effective strategy in areas with a short malaria transmission season. The intervention considers treatment with SP +AQ for four rounds (four months) through the rainy season (July to Oct) for children 3-59 months old from current coverage levels of 22 percent of children (approximately 100,000 children) to 90 percent (approximately 500-600,000 children).
Implementation Considerations
Expansion of SMC to these levels would require significant planning and human resources. The Northern region of Ghana is large and in some areas sparsely populated with poor road infrastructure. Expanding to these levels would require GH¢ 17 million initially rising to GH¢ 29 million by 2030 (2018 GH¢).
Costs and Benefits
Costs
The costs for this intervention are drawn from a study in Northern Ghana which suggests a unit cost of GH¢ 43 per child per course of SMC. For a targeted increase in coverage to 90 percent, the total cost of SMC is, therefore, GH¢ 17 million initially rising to GH¢ 29 million by 2030 (2018 GH¢). The present value of this is GH¢ 167 million at an 8% discount rate.
Benefits
The intervention would avoid 964,000 uncomplicated cases, 72,400 severe cases and 3,265 deaths between 2018 and 2030. This is valued at GH¢ 116 million initially rising to GH¢ 496 million by 2030 (2018 GH¢). The present value of this is GH¢ 2,303 million at an 8% discount rate.
Intervention 3: (Near) Universal Testing and Treatment of Suspected Cases Presenting at Health Facilities
Overview
The WHO recommends diagnostic testing to confirm malaria before providing anti-malarial treatment to suspected cases. This recommendation aims to limit indiscriminate anti-malarial use, and is premised on the emerging parasitic resistance to antimalarials; the quest to have clinicians find treatments that are appropriate for non-malaria febrile illness; declining malaria transmission in previously high transmission areas; and increased availability of diagnostics, notably, rapid diagnostic tests (RDTs) for malaria in resource-limited environments.
Currently, testing coverage of suspected malaria cases in health facilities is 90 percent, and the analysis investigates movement towards (near) universal testing as per NMCP targets. The specific intervention analyses increasing the probability of being tested and diagnosed for clinical malaria infection for suspected cases presenting at health facilities before treatment of all confirmed cases of clinical malaria across Ghana - a 10 percent increase (to almost 100 percent coverage) in the probability of being tested with an RDT or by microscopy in all three zones.
Implementation Considerations
To initiate this intervention would require a number of steps. These include i) training, to ensure health facility staff use tests and are aware of appropriate protocols for the use of tests ii) improvements in availability of RDTs or microscopy testing equipment, including minimizing stock-outs, particularly in remote areas and iii) monitoring and evaluation to detect areas of deficiency and constraints to reaching near-universal coverage.
Costs and Benefits
Costs
A previous study indicates that the average cost of implementing RDT (training, supervision and the provision of RDT itself) in a standard-setting is GH¢ 24.9 per suspected patient in 2018 values. However, due to the envisioned difficulty in ensuring test-based diagnosis in the remaining 10 percent of suspected malaria cases, this paper suggests a ‘last-mile’ premium of 10x, i.e. reaching the last 10 percent will cost ten times the average cost of reaching the first 90 percent – a value of GH¢249 per suspected case. Under this assumption, the costs are equal to GH¢7 million in the first year, increasing to GH¢ 14 million by 2030. The total costs are GH¢ 87 million between 2018 and 2030 at an 8% discount rate.
Benefits
By properly diagnosing malaria using tests and treating early, the intervention will avoid a large number of severe malaria cases - 434,780 between 2018 and 2030. In turn, this is expected to avoid 24,700 deaths over the same time period. There will also be a modest reduction in uncomplicated malaria cases (17,330 in total to 2030) well as some cost savings in drugs and time from improved diagnosis equal to GH¢ 17 per suspected malaria case. Overall the benefits are GH¢ 211 million in the first year, rising to GH¢ 2,689 million by 2030. The total present value of benefits over the time period are GH¢ 11,595 million of which 99% are attributable to avoided mortality.