Ghana Priorities: Mental Health
Technical Report
The Problem
With a population of nearly 30 million people, WHO estimates that approximately 13% of the population in Ghana suffer from a mental disorder, of which 3% suffer from a severe mental disorder and the other 10% suffer from a moderate to mild mental disorder (WHO, 2007). However, there is a lack of reliable data regarding the prevalence of mental and neurological disorders in the country. Mental disorders are a leading cause of years lived with disability in Ghana, behind iron-deficient anaemia (IHME, 2013a). Among patients seeking treatment for mental health issues, schizophrenia, substance abuse, and mood disorders are the top three diagnoses, although a large percentage of people receive no specific diagnosis. Recent estimates by Ritcher and Roser (2018), indicate that the average prevalence of depression, anxiety disorders and schizophrenia over the period 1990 to 2017 are 3.3%, 2.9% and 0.17%, respectively. The treatment gap for mental health disorders in Ghana is estimated to be more than 98% (WHO, 2007).
Though studies have estimated the costs of mental illness in Ghana, there is paucity of studies assessing the cost-benefit of interventions targeting mental health. With the country transitioning from low-income to middle-income status leading to reductions in official development assistance (Nonvignon et al., 2018), and the Ministry of Health institutionalizing health sector priority setting in Ghana (Hollingworth et al., 2019), the analyses of benefit-cost could inform both health sector and general country-level policy decisions relating to priority setting. Hence, this study evaluates the benefit-cost of interventions targeting screening and treatment of depression, anxiety disorders and schizophrenia.
Intervention 1: Screening and Treatment of Depression
Implementation Considerations
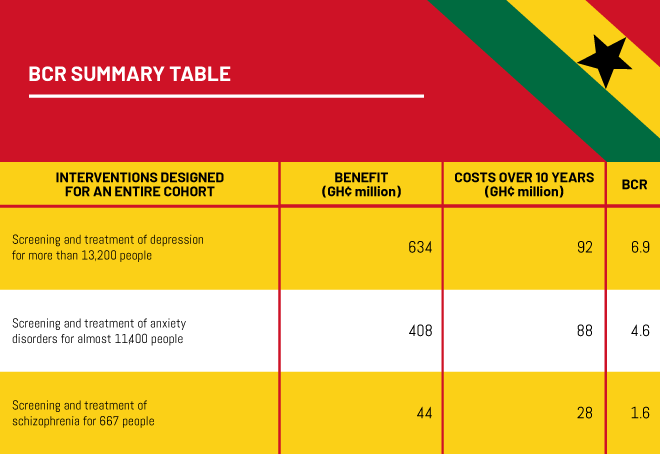
The number of people in Ghana projected to receive treatment for depression within the cases identified is estimated to be about 13,202. It is projected that about 30% (3,961) of those who receive treatment will remain on antidepressants for life.
Costs
Projected total cost for depression was estimated at approximately GHS 110.3 million with indirect cost of treatment constituting 16.2% of total cost for the entire period of 10 years without discounting. The projected discounted total cost for depression is estimated to be approximately GHS 98.2 million, GHS 92.3 million and GHS 82.5 million at 5%, 8% and 14% discount rates, respectively. Direct non-medical cost constituted 45.5% of the total projected cost. Direct medical cost and indirect cost constituted 38.3% and 16.2% of the remaining cost, respectively.
Benefits
The total expected benefits through the impact of a depression programme on employment is estimated at GHS 948 million. The programme benefits in terms of patient productivity loss was relatively higher estimated at GHS 565 million compared to caregiver’s benefits derived from caregiver productivity loss also estimated at GHS 271 million. Discounting expected benefits at 5%, 8% and 14% rates, benefits derived were estimated at GHS 730 million, GHS 634 million and GHS 492 million respectively. Self-harm and suicide averted due to a depression programme is estimated at GHS 23 million and GHS 87 million respectively.
Intervention 2: Screening and Treatment of Anxiety Disorder
Implementation Considerations
The number of people in Ghana projected to receive treatment for anxiety disorder within the cases identified is estimated to be about 11,362. Similar to the depression case scenario, it is projected that about 30% (3,409) of those who receive treatment will remain on antidepressants for life.
Costs
The projected total cost for anxiety disorder was estimated at approximately GHS 108.3 million with indirect cost of treatment constituting 20.6% of total cost for the entire period of 10 years without discounting. The projected discounted total cost for anxiety disorder is estimated to be approximately GHS 95.1million, GHS 88.7million and GHS 78.3million at 5%, 8% and 14% discount rates respectively. Direct non-medical cost constituted 39.8% of the total projected cost. Direct medical cost and indirect cost constituted 39.6% and 20.6% of the remaining cost, respectively.
Benefits
An intervention programme targeting anxiety disorder results in an estimated total benefit of GHS 610 million. When discounted at 5%, 8% and 14% rates, benefits derived were estimated at GHS 470 million, GHS 408 million and GHS 316 million respectively. Self-harm and suicide averted due to anxiety disorder programme is estimated at GHS 20 million and GHS 63 million respectively. The programme benefit in terms of patient productivity loss is estimated at GHS 292 million.
Intervention 3: Screening and Treatment of Schizophrenia
Implementation Considerations
The number of people in Ghana projected to receive treatment for schizophrenia within the cases identified is estimated to be about 667. Schizophrenia patients receive treatment for life.
Costs
The projected total cost for schizophrenia was estimated at approximately GHS 36 million with indirect cost of treatment constituting 12.5% of total cost for the entire period of 10 years without discounting. The projected discounted total cost for schizophrenia is estimated to be approximately GHS 30.6 million, GHS 28.2 million and GHS 24.4 million at 5%, 8% and 14% discount rates respectively. Direct non-medical cost constituted 24.3% of the total projected cost. Direct medical cost and indirect cost constituted 63.2% and 12.5% of the remaining cost respectively
Benefits
The expected benefit of schizophrenia programme was estimated at GHS 66 million. The programme benefit in terms of patient productivity loss estimated at GHS 43 million and GHS 17 million to caregivers. Self-harm and suicide averted due to a schizophrenia programme is estimated at GHS 1 million and GHS 4 million respectively.