Ghana Priorities: Maternal and Child Health
Technical Report
The Problem
Over the last three decades, Ghana has invested large amounts of effort in implementing various strategies to reduce maternal and child mortality in the country. Among the key interventions are: Safe Motherhood Program (SMP), Life-Saving Skills (LSS) program, Integrated Management of Childhood Illness (IMCI), Community-Based Health Planning and Services (CHPS), User Fees Exemption for Delivery (UFED), Focused Antenatal Care (FANC), National Health Insurance Scheme (NHIS), and Accelerated Child Survival and Development (ACSD).
These programs have led to significant improvements in maternal and child health over time. However, Ghana failed to meet the Millennium Development Goal 4 and 5 targets regarding reduction in child and maternal mortality by the end of the year 2015 when the era of the MDGs closed out (United Nations, 2015). Under-five and infant mortality in Ghana decreased from 155 and 77 deaths per 1,000 live births in the year 1988 to 52 and 37 per 1,000 live births in 2017 respectively (Ghana Statistical Service, 2018).
While the maternal mortality ratio was reduced from 760 per 100,000 live births in the year 1990 to 310 per 100,000 live births by the year 2017, this ratio is still significantly higher than the MDG 5 target of 190 maternal deaths per 100,000 live births (United Nations, 2015; Ghana Statistical Service (GSS); Ghana Health Service (GHS); ICF International, 2018).
Ghana failed to meet the required reductions in maternal and child mortality in spite of many initiatives targeted at reducing mortality that has been implemented in the country. There is, therefore, the need to identify and implement additional proven cost-effective interventions with comparatively high impact in order to accelerate improvements in maternal and child health in the country. We present in this paper the benefit-cost analysis of three strategic health systems strengthening interventions that have shown enormous potential for improvement of maternal and child health in Ghana. These interventions are the Ghana Essential Health Intervention Project (GEHIP), the NEWborn Health Intervention Study (NEWHINTS) and Emergency Obstetric and Newborn Care (EmONC).
Intervention 1: Ghana Essential Health Intervention Project (GEHIP)
Overview
GEHIP was a five-year plausibility trial designed to strengthen the health system by promoting the delivery of quality primary health care services. It is best understood as a bundle of related interventions targeting each of the six WHO health system building blocks (World Health Organization, 2010). The specific activities were: improving leadership capacity development, promotion of grass root political and community engagement, information for decision-making, budgeting, logistics, training, and health worker deployment, community-based primary healthcare scale-up and the provision of health services at community locations (Awoonor-Williams et al., 2013; Bawah et al., 2019; Kanmiki et al., 2019).
Implementation Considerations
- Series of training programs for district level health care managers and frontline healthcare providers on leadership, stakeholder engagements for health delivery at the community level, training on how to deal with the lead causes of maternal and neonatal deaths including neonatal resuscitation, WHO recommended care for the newborn (World Health Organization, 2013).
- Mentorship and monitoring support to frontline healthcare providers on how to leverage resources from communities and other stakeholders to improve healthcare delivery and health-seeking
- Flexible funding of up to US$ 0.80 dollar per capita for district-level prioritization of healthcare needs activities
- Community-based low-cost emergency referral system that involved the promotion of facility-based delivery, effective communication and a process of convening community engagement for sustaining social support for referral operations.
Costs and Benefits
Costs
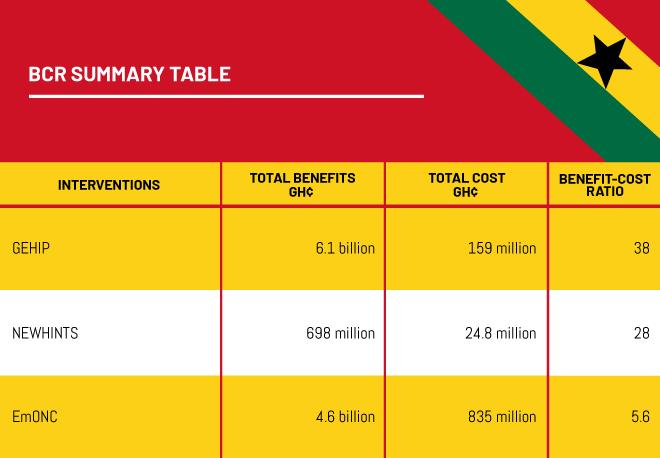
The cost of the GEHIP’s intervention is the sum of all six category costs namely the cost of capacity building among human resources for health through trainings and reorientation, the cost associated with additional health service delivery, the cost related to additional medicines and vaccines, health information, leadership/governance-related expenditures and other costs that mainly involved the program costs of deploying a community-based emergency transport system. Since the GEHIP project was implemented over a three-year period, the total for these categories over the three years is summed up to represent total implementation costs of GEHIP. As GEHIP trial covered 6.8% of Ghana’s rural population, these costs were then scaled up to 100% nationwide coverage of the rural population of Ghana, bringing total costs to GH¢ 84.0 million for the year 2018. These costs were then modeled over a six-year period (2018-2023), resulting in a total cost for the six-year period of GHC 159 million at an 8% discount rate.
Benefits
Baseline and end-line survey data from the GEHIP project and comparison districts were used to estimate the incremental health benefits of GEHIP. The difference-in-differences empirical approach was used to estimate the number of newborn lives saved as well as under-five morbidity reductions for two disease conditions (malaria and diarrhea cases).
One of the key impacts of the GEHIP project was a sharp reduction in neonatal deaths over the first three years (Bawah et al, 2019) with declining impacts thereafter. Out of the possible 71,990 expected neonatal deaths over the period 2018-2025, we expect GEHIP would save the lives of 7,551 neonates. Valuing these deaths at Ghana Priorities assumptions value per death averted per year puts the economic value of these averted deaths at GH¢ 5.8 billion.
Also, GEHIP was found to reduce the incidence of diarrhea and malaria among under-fives by 37% and 25% respectively. Using information on the projected number of under-fives in rural Ghana, we estimate the total economic benefits of GEHIP on malaria and diarrhea cases avoided to be GH¢ 295.2 million based on estimates of the total days of illness avoided, hospital treatment cost per case, and productivity loss due to time lost by parent in seeking care for her under-five child. Thus, the total economic value of GEHIP benefit is the sum of economic benefits from mortality and morbidity reduction which is GH¢ 8.3 billion; GH¢ 6.1 billion and GH¢ 5.4 billion, using discount rates of 5%, 8%, and 14%, respectively.
Intervention 2: NEWborn Health Intervention Study (NEWHINTS)
Overview
The NEWHINTS intervention involves the training of lay community health workers called community-based surveillance volunteers (CBSV) to identify pregnant women in their communities and to do two home visits during pregnancy and three visits on days 1, 3, and 7 postpartum. The goal is to improve delivery, newborn care practices and care-seeking for mothers and sick newborn babies with an overall aim of reducing maternal and child mortality (Kirkwood et al., 2010).
Implementation Considerations
- Training of Community-based Service Volunteers (CBSV) including periodic refresher trainings
- Monitoring and supervision system at the district level to ensure conformity to guidelines and protocols
- Due to high attrition of CBSVs systems are put in place for periodic/occasional replacement of CBSV
- NEWHINTS intervention works best in places where the community-based health planning and services program (CHPS) is functioning properly
- Improving the capacity of health staff in essential newborn care in health facilities is necessary to ensure optimal benefits from the intervention
Costs and Benefits
Costs
The total cost of this intervention if expanded to cover 100% of Ghana’s rural population would be GH¢ 24.9 million per year. This is made up of the summation of six categories of cost items as published by Pitt et al (2016). These are capital cost, human resources, meetings and trainings, supplies, overheads and maternal related costs (the opportunity cost to mothers receiving the intervention) (Pitt et al., 2016).
Benefits
The NEWHINTS intervention was found to reduce neonatal mortality by 8%. This would translate into about 819 neonatal deaths averted per year if scaled up to the rest of rural Ghana. At an economic value of 12,854 per life saved, the economic value of this reduction is estimated at GH¢ 667 million.
NEWHINTS is estimated to reduce not only mortality but also morbidity. Since we do not have information on morbidity reduction, we estimate an additional 2% reduction in mortality and attribute this to morbidity reduction. These result in the economic value of morbidity reduction to be GH¢ 30.3 million. Hence, the total benefits of NEWHINTS intervention are estimated at GH¢ 698 million.
Intervention 3: Emergency Obstetric and Neonatal Care (EmONC)
Overview
Emergency obstetric and neonatal care (EmONC) is known to be a high impact intervention highly recommended for improving maternal and neonatal health outcomes in resource-poor settings (Adam et al., 2005). The provision of Basic (BEmONC) alone is estimated to avert up to 40% of intrapartum-related neonatal mortality and have a significant impact on maternal mortality as well (Lee et al., 2011).
Implementation Considerations
According to the Ghana national standards for EmONC, there should be at least 5 EmONC facilities per 200,000 population. Our cost estimates are based on the estimated number of EmONC facilities required to fill the gap using gap analysis from the 2011 EmONC survey in Ghana (Ghana Ministry of Health, 2011).
Costs and Benefits
Costs
We did not find any prior study in Ghana that has conducted a cost analysis of EmONC provision. Therefore, we rely on an EmONC costing study conducted in Tanzania involving 6 facilities (Mengistu et al., 2019). Ten categories of cost items were specified to make up the total cost of EmONC provision according to the referred study. As per the last Ghana national assessment for emergency obstetric and newborn care survey conducted in 2011, the gap in comprehensive EmONC services is 472 health facilities (Ghana Ministry of Health, 2011). Drawing from Mengistu et al’s EmONC costing of 6 health facilities, and projections over a 15-year period (2018-2032) it would cost a total of GH¢ 835 million at 8% discount rate to fill the national gap in EmONC facilities in Ghana. These cost estimates do not envisage the building of hospitals/facilities from scratch. Instead, the analysis takes into account hospitals and other health facilities that already exist but which lack the logistical and human capacity to provide EmONC services. So cost estimates are based on filling this logistical and capacity needs of staff including minor extension/renovation of already existing buildings.
Benefits
The benefit estimates are drawn from Gabrysch et al 2019 which found that EmONC achieves 27% reduction in neonatal mortality. Based on this, the estimated projected economic benefits accruing from neonatal deaths avoided and morbidity reduction by scaling up EmONC to the whole country is GH¢ 5.8 billion.