Ghana Priorities: Family Planning
Technical Report
The Problem
Unplanned pregnancies, including teenage pregnancy, perpetuated by low demand for, and lack of access to family planning are linked with higher risks of birth complications such as maternal deaths and early child deaths, and malnutrition in children under-five. Access to contraception is therefore a key strategic lever for development. Contraception affords women the opportunity to adequately space their children, further their own education and that of existing children, enter the workforce, improve the nutritional profile of household members, among other things. Securing access to family planning services therefore remains a critical component of building human capital in most developing countries.
In 2015, Ghana mounted a family planning program which had as its objective to increase the contraceptive prevalence rate (CPR) of married women aged 15-49 from 22.2 to 29.7 percent, and that of unmarried women from 31.7 to 40 percent by 2020 (GFPCIP, 2015). The implementation of the program has been successful, the CPR is 30.8 percent for married women (compared with 22.2 in 2014 before the program) and 38.4 percent for unmarried women compared with 31.7 in 2014 (Ghana Maternal Health Survey 2017). These represent an annual average increase in CPR by 2.9 percentage points for married and 2.2 percentage points for the unmarried. However, survey data suggests that there remain a significant percentage of women with an unmet need for contraception.
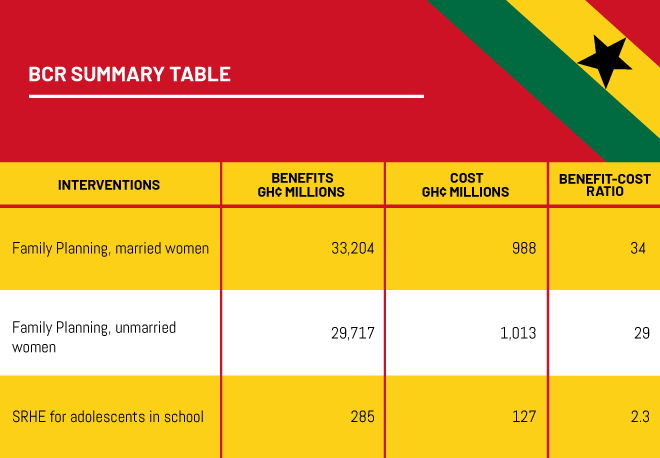
This first intervention makes the investment case for an extension of the current programme (post 2020) by demonstrating that the economic and health benefits far exceed the costs of the programme.
Likewise, the relevant information and the unavailability of family planning commodities to adolescents, places teenage childbearing in Ghana higher than the global average. According to UNICEF, In 2018, the estimated adolescent birth rate globally was 44 births per 1,000 girls aged 15 to 19; in West and Central Africa, this figure stood at 115 births, the highest regional rate in the world; in Ghana, it is 75 (MICS 2017/18). Children of teen mothers run the risk of high morbidity and mortality. Teen mothers are more likely to have adverse pregnancy outcomes and are less likely to continue with their education, thus pushing them (and their children) into poverty.
Sexual and reproductive health education does form part of the curriculum in Ghana, and approximately 77 percent of adolescents are exposed to sex education by the time they complete Senior High school (Awusabo-Asare, 2017). However the coverage of topics is minimal, and drop out rates are considerable for Junior (40%) and Senior High school (20%). Exposure to adequate comprehensive sex education is needed for adolescents to have a good understanding of their reproductive health and appropriate adaptive behavior to maintain adequate sexual and reproductive health.
The second intervention analyzed here demonstrates that compulsory, comprehensive, and universal (boys and girls) sexual reproductive health education, as well as the provision of contraceptives, is also a beneficial intervention.
Intervention 1: Increase the CPR by 10 pp for married women; 12 pp for unmarried women
Overview
The intervention proposed here makes the investment case for an extension of the current programme, with an increase in CPR targets: In phase 2, a five-year programme targeting increase in the CPR from 29.7% to 40% for married women and a six-year programme targeting an increase in the CPR from 38% to 50% for unmarried women. A 2% annual increase in the contraceptive prevalence rate (CPR) is modeled, based on the Government of Ghana’s past performance.
Of the estimated 7.4 million women between the ages of 15 and 49, 4.2 million are married, and the number of annual unintended pregnancies per year is 292,700, of which 81,500 are avoided by the intervention.
Of the 3.2 million unmarried women (never-married and divorced/separated), the number of unintended pregnancies is approximately 220,800 per year, of which 71,600 are avoided by the intervention.
Costs and Benefits
Costs
The costs that we consider are activity costs, commodity and direct consumables, indirect costs (consisting of the cost of transportation to health facilities as well as time spent at health facility to receive FP service), and the cost of side effects. The activity cost, US$5.52 per woman targeted, covers demand creation and service delivery. It also includes all direct point-of-service costs. The costs of family planning commodities and direct consumables is US$3.74 per actual user as computed in GFPCIP (2015) and include a variety of additional loaded costs for each commodity (e.g., freight, insurance, customs and clearing charges, warehousing, and distribution fees to the last mile). Financing, policy and enabling environment, management and accountability were components of the programme, as it was implemented in 2015, but the health infrastructure having been reinforced as a consequence of the first phase, these components are not considered additional to the second phase. The exchange rate, GHS per USD is 4.56.
The indirect costs of family planning consider transport costs and the opportunity cost of time and have been valued at GHS101 per user. It is assumed that users visit a health facility/doctor four times per year.
The percentage of women experiencing side effects ranged from 9 to 11% according to the DHS. It was assumed that, while the side effects from contraception may be experienced for some portion or throughout the duration of the contraceptive period, there is only one visit to the FP provider, valued at GHS101 per user.
Below are the cost components for both married and unmarried women.
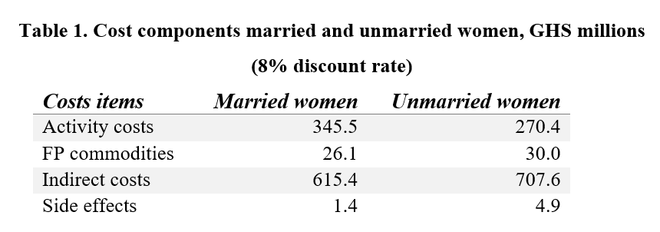
Total discounted costs (8%) are GHS 988.5 million for married; GHS 1,012.9 million for unmarried. Note that short-term costs and benefits are modeled over a 6-year and 8-year period respectively for married and unmarried women with an assumed 2pp increase in CPR per year. The longer time frame for the intervention targeting unmarried women is required because there is a larger assumed total increase in CPR among unmarried women (12 pp increase vs 10pp for married women), and the average time for contraceptive use is longer among unmarried women (3 years for unmarried women and 2 years for married women).
Benefits
The anticipated benefits of increasing the CPR by 10 and 12 percentage points for married and unmarried women, respectively, include maternal and infant deaths averted, pregnancy and induced abortion costs avoided, and the demographic dividend that results from a decrease in the dependency ratio.
The maternal mortality rate, which includes death during delivery and 2 months post delivery, is 310 per 100,000 live births (Ghana Maternal Health Survey 2017). Approximately 25 maternal deaths are averted for every 2% increase in the CPR for married women; 12, for unmarried. Each maternal death leads to 38.2 life years gained. Maternal mortality averted among married women is valued at GHS 240 million over 6 years; among unmarried, GHS 189 million over 8 years.
The causes of neonatal mortality are, unfortunately, numerous and vary greatly. It was decided to use the infant mortality rate associated with inadequate spacing. Failure to space live birth at least 24 months apart has a current mortality rate of 36 per 1000 live births; the risk ratio of neonatal mortality from lack of spacing is 1.26. Approximately 47 and 23 neonatal deaths are averted per 2% increase in the CPR for married and unmarried women, respectively. Life expectancy being 63.5 years at birth, total neonatal mortality has been valued at GHS 742.1 million (married) over 6 years, and GHS 582.8 million (unmarried) over 8 years.
Since the intervention is anticipated to avert 81,500 and 71,600 pregnancies for married and unmarried women, respectively by the end of the program, there is a benefit associated with the avoided costs of antenatal care, delivery and newborn costs. Another benefit is avoided abortions. The percentage of unwanted pregnancies aborted is 11.6%, an average across the age groups 15-49 (Ghana Maternal Health Survey, 2017). It is estimated that raising the CPR averts approximately 4,725 and 2,769 abortions among married and unmarried women, respectively by the end of the program timeline. These benefits are relatively minor, valued at GHS 34.9m and 25.7m respectively for married and unmarried women.
What is the impact of a 10% increase in CPR on the current TFR of 3.9? Using Ghana, among other countries, as a case study, Bongaarts (2017) theorizes that a 1% increase in the CPR leads to a 0.054 decline in the TFR. For married women, holding all things equal including the fertility rate of unmarried women and adolescents, the TFR declines to 3.59 as a result of 10% in CPR. For unmarried women, a 12% increase in the CPR causes the TFR to decline to 3.62.
The socioeconomic impact that a decline in TFR has on the economy is what is referred to as the demographic dividend. Ashraf et al. (2013), using Nigeria as an example, postulates that a reduction in TFR by 0.5 leads to 5.6 percent increase in GDP per capita over 20 years. This translates into a proportional increase of 3.45% and 3.12% of GDP per capita over 20 years, associated with the increase in CPR for married and unmarried women respectively. As is evident below, the demographic dividend benefit is the largest category of benefit, comprising 97% of the total benefit.
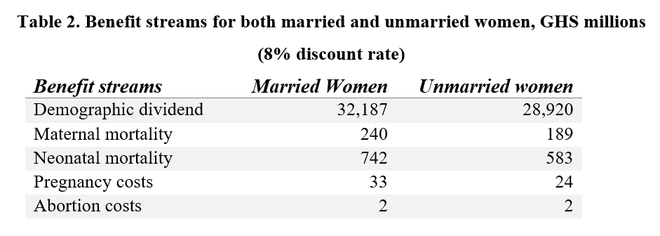
Total discounted benefits (8%) are GHS 33,204 million and GHS 29,717 million for interventions targeting married and unmarried women, respectively.
Intervention 2: Universal compulsory sexual and reproductive health education (SRHE) for both boys and girls, 15-19 years; (re) training School-Based health coordinators; provision of male contraceptives
Overview
According to Darroch et al. (2016), the percentage of African girls who had ever had sex by age 16 was 27%; whereas, by age 19, it was 66%. Slightly more than one-third of the adolescents who had ever had sex (32% of the males and 39% of the females) reported that the first sexual intercourse was unplanned. Furthermore, although virtually every adolescent interviewed had heard of contraceptives, the proportion that used a method to prevent pregnancy at first or last sexual activity was lower: 46% of the males and 49% of the females. The unmet need for contraception among Ghanaian adolescents indicates that more information needs to be transmitted to adolescents: 95% of sexually active adolescent females, who are unmarried, want to avoid pregnancy within the next two years, but 62% have an unmet need for family planning. The evidence suggests that an intensive intervention that targets adolescents at the junior and senior high school levels and responds to their contraceptive needs would be a key element in re
versing the high rate of unwanted pregnancies in Ghana.
The Ghana Adolescent Reproductive Health Policy (2000) adopted a multisectoral approach to addressing adolescent reproductive health issues. The policy explicitly encouraged and led to the inclusion of a reproductive health component in the educational curriculum at the primary, junior high and senior high school levels. In 2013, the National HIV and AIDS, STI Policy advocated for the inclusion of age appropriate SRH education in the school curriculum, which includes lessons on HIV/AIDS and other STIs for girls, 10-19 years.
However, given the fact that certain core themes are electives and girls are the principal beneficiaries because certain subject matters have been combined with home economics courses and the like, the intervention proposed here is universal (boys and girls), comprehensive, and compulsory SRHE, throughout JHS and SHS, a revision of the curriculum, the (re)training School-based health coordinators, and the distribution of contraceptives (i.e. condoms).
The number of unintended pregnancies, and hence dropouts, at some point during JHS is estimated to be 56,300; 24,900 at SHS level.
The intervention is modeled over 7 years: the first year assigned to revision of curriculum and retraining; the following six years represent the movement of one cohort through JHS and SHS, three years each.
Costs and Benefits
Costs
The costs of the intervention are:
Curriculum adaptation, retraining and delivery. We relied on per unit estimates from the costing estimates by the GFPCIP. The cost per student is $8.73 (2015). The cost of a similar activity in Nigeria was estimated to be $6.84 in 2011 (Kivela et al, 2013).
Cost of FP commodities. This was costed in the GFCPCIP at $3.74 per user (2015).
Cost of additional years of schooling. The total (direct and indirect) cost of education was estimated at GHS 1184 per student, per year (Results for Development, 2015). The opportunity cost of education was also included here and was based on what is considered the next best alternative available to minors, who are not attending school. The national child labour rate being 30%, this figure was taken as an estimation of the number of dropouts who would be able to secure employment, using the mean wage for those without/primary education (Turkson et al, 2019) of GHS 5119.
Recurrent costs were assumed to be 10% of annual programme costs.
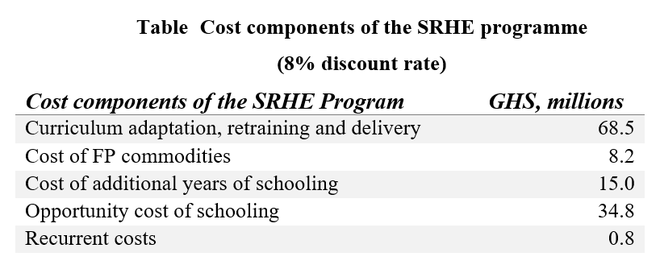
Total discounted costs (8%) are GHS 127 million.
Benefits
In order to arrive at the number of unintended pregnancies avoided by the intervention, a review of the literature of randomized trials discovered that the relative effect of SRHE interventions was an increase in birth control methods (specifically condoms) by 18%. It is assumed that the use of birth control averts pregnancy. Therefore the number of unintended pregnancies avoided by the intervention is 10,140 at the JHS level and 4480 at SHS level.
It is assumed that contraceptive use by sexually-active adolescents delays pregnancy to an age when it is physically safer to have children. Therefore all benefits should be considered as relative to pregnancy at an older age. The anticipated benefits from delayed pregnancy include avoided medical costs of birth, fistula, caesareans and abortions, infant and maternal mortality, and the marginal income gain from completed JHS and SHS.
- The avoided medical costs associated with antenatal care, pregnancy and delivery are estimated at GHS 266 and include direct and indirect costs.
- Cesareans make up 16% of all births, and early pregnancy increases this risk by 80% (Yussif et al. 2017). The medical cost of a caesarean is estimated at GHS 3000.
- The prevalence of induced abortions for mothers who are less than 20 years of age is 18.8%, and adolescent mothers are 86% more likely to have an induced abortion (Ghana Maternal Health Survey, 2017). The medical cost of abortion is assumed to be approximately GHS 425 in Ghana.
- The maternal mortality for all women is 310 per 1000 women, but 510 per 1000 women for adolescent girls, an increased risk of .20% (Nove et al. (2014). Approximately 9 deaths would be averted per cohort.
- According to the Ghana Maternal Health Survey (2017), among adult women, the incidence of infant mortality is 27 per 1000 births, but the pregnancies of adolescent women are 30% more likely to result in the death of the infant. Approximately 118 infant deaths would be averted due to the intervention.
- Lastly, around 1.6 per 1000 births lead to obstetric fistula in women (Ghana Health Service, 2015), while for adolescents the risk is 28% higher (Tebue et al 2012).
The value of maternal and child lives saved follows standard protocols throughout the Ghana Priorities project, and assumes each adolescent maternal life saved avoids 53 years of life lost (YLL), each child life saved avoids 64 YLLs and each YLL is valued at around GHS 13,000 increasing with GDP per capita growth (Wong and Dubosse, 2019). Fistula is assumed to lead to a life-long disability that remains untreated, and the disability weight for untreated fistula is 0.346 years lost to disability (YLD) per year (Higashi et al. 2014). Each YLD avoided is valued at the same as each YLL avoided.
Lastly, with respect to continued education, benefits are valued as the marginal lifetime income gain associated with increased education attainment. The marginal increase in wage for a year of JHS is GHS 666 per year and for SHS is GHS 896, based on Mincerian equations estimated from GLSS 7 data and documented in another paper in the Ghana Priorities series (Turkson,, et al., 2019). This increased wage value per year is assumed to increase with real income per capita growth, and lasts for the entirety of the women’s working lives. In two of the interventions, the increase in wages associated with more education is the largest benefit.
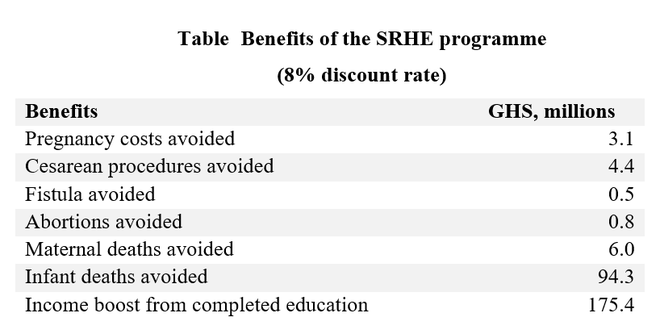
Total discounted benefits (8%) are GHS 285 million.
The BCR for unmarried women is slightly lower, despite the fact that the intervention models a 12 percentage point increase in the CPR, as opposed to 10 for married women. There are, in fact, fewer unmarried women (43% of all women ages 15 - 49), who have a preference for long-term contraception, and it is assumed that contraceptive adherence lasts for an average of three years. This results in increases in both the FP commodity costs and the indirect costs associated with visiting a service provider. Furthermore, the increase in the CPR for married women has a greater impact on the population total fertility rate, declining from 3.9 to 3.59; whereas, it declines to 3.62 for unmarried women. This bears on the demographic dividend estimation, which constitutes over 90% of benefits.