Cost-effectiveness of Maternal and Newborn Health Interventions
Assessment Paper
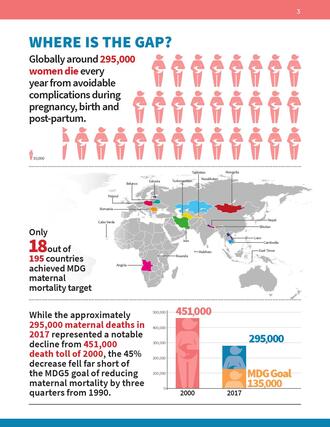
 Maternal health has long been a stated priority in a variety of global goals and strategies: the Millennium Development Goals, the Sustainable Development Goals, FP2020, and the Global Strategy for Women’s Children’s and Adolescents’ Health. However, many of the goals have not actually been achieved, specifically those around reducing the number of maternal deaths – the deaths of women during pregnancy, childbirth, and up to 42 days post-partum. While the approximately 295,000 maternal deaths in 2017 represented a notable decline from the 2000 death toll of 451,000, the 45% decrease fell far short of the MDG5 goal of reducing maternal mortality by three quarters from 1990. The United Nations (UN) estimated that only 9 countries, out of the 95 being monitored, had reached their individual maternal mortality reduction goals by 2015. Since then, it is estimated that only 9 more countries have achieved their individual goals, although this is uncertain given the lack of an updated 1990 estimate from 2015.
Maternal health has long been a stated priority in a variety of global goals and strategies: the Millennium Development Goals, the Sustainable Development Goals, FP2020, and the Global Strategy for Women’s Children’s and Adolescents’ Health. However, many of the goals have not actually been achieved, specifically those around reducing the number of maternal deaths – the deaths of women during pregnancy, childbirth, and up to 42 days post-partum. While the approximately 295,000 maternal deaths in 2017 represented a notable decline from the 2000 death toll of 451,000, the 45% decrease fell far short of the MDG5 goal of reducing maternal mortality by three quarters from 1990. The United Nations (UN) estimated that only 9 countries, out of the 95 being monitored, had reached their individual maternal mortality reduction goals by 2015. Since then, it is estimated that only 9 more countries have achieved their individual goals, although this is uncertain given the lack of an updated 1990 estimate from 2015.
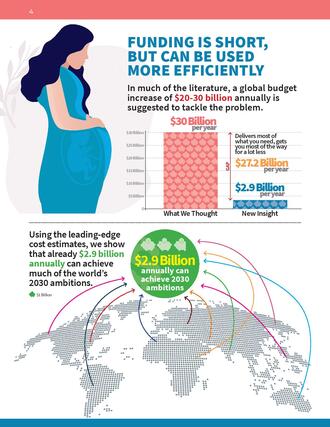
 A new report by global health experts Ingrid K. Friberg and Eva Weissman for Copenhagen Consensus, supported by funding from Merck for Mothers*, attempts to add novel presentations of cost efficiency and impact to the discourse on maternal and child health. It situates this discourse within the context of limited budgets and finite resources; a reality for the vast majority of countries that struggle to end preventable maternal deaths. While similar costing exercises have been conducted, the findings and funding demands have placed the achievement of strong maternal health beyond the reach of many low- and middle-income countries. Moreover, there remains an unclear understanding of how the indirect costs, opportunity costs, and outcomes, between various Maternal and Newborn Health (MNH) packages of services, compare. This report seeks to bridge that knowledge gap, providing a direct head-to-head comparison between multiple MNH interventions and packages, while also focusing on a subset of countries with the heaviest burden and highest investment need.
A new report by global health experts Ingrid K. Friberg and Eva Weissman for Copenhagen Consensus, supported by funding from Merck for Mothers*, attempts to add novel presentations of cost efficiency and impact to the discourse on maternal and child health. It situates this discourse within the context of limited budgets and finite resources; a reality for the vast majority of countries that struggle to end preventable maternal deaths. While similar costing exercises have been conducted, the findings and funding demands have placed the achievement of strong maternal health beyond the reach of many low- and middle-income countries. Moreover, there remains an unclear understanding of how the indirect costs, opportunity costs, and outcomes, between various Maternal and Newborn Health (MNH) packages of services, compare. This report seeks to bridge that knowledge gap, providing a direct head-to-head comparison between multiple MNH interventions and packages, while also focusing on a subset of countries with the heaviest burden and highest investment need.
For key findings download the brochure "How to save more mothers per dollar spent" here.
Highlights
 The key findings of this report are based on a foundational understanding that there is no magic bullet to reducing maternal mortality. A genuine commitment to MNH demands a healthcare system that has the capacity to respond to MNH needs across the spectrum, at all stages. In order to know where and how to best invest in strengthening MNH health systems in low and middle-income countries, knowing which of those options are the most cost-efficient helps those with limited budgets narrow the focus of their efforts – placing resources and energy in the areas where they stand to make the greatest impact. The analysis undertaken shows that the strongest investments in maternal and newborn health within low- and middle-income countries are in the following areas.
The key findings of this report are based on a foundational understanding that there is no magic bullet to reducing maternal mortality. A genuine commitment to MNH demands a healthcare system that has the capacity to respond to MNH needs across the spectrum, at all stages. In order to know where and how to best invest in strengthening MNH health systems in low and middle-income countries, knowing which of those options are the most cost-efficient helps those with limited budgets narrow the focus of their efforts – placing resources and energy in the areas where they stand to make the greatest impact. The analysis undertaken shows that the strongest investments in maternal and newborn health within low- and middle-income countries are in the following areas.
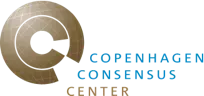
Basic Emergency Obstetric and Newborn Care (BEmONC)
Providing $61.50 worth of benefits for every $1 dollar spent by governments and beneficiaries, the package of interventions with the third-highest BCR is BEmONC. This would require an additional $2.2bn per year in investments, and would lead to an expected additional 93,000 avoided maternal deaths, 0.87m avoided newborn deaths and 0.81m avoided stillbirths.
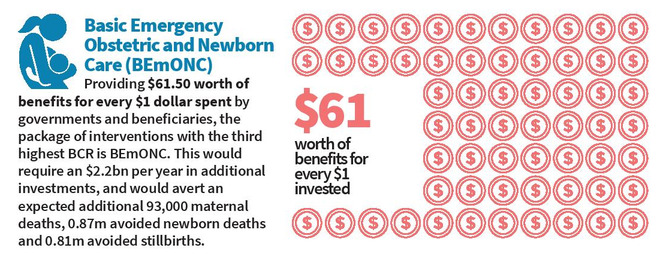
Safe & Inclusive Family Planning
Providing $26.80 worth of benefits for every $1 dollar spent by governments and beneficiaries is the sole intervention (as opposed to a package) with the greatest absolute impact on maternal deaths. Scaling up this intervention to meet 90% of unmet need in the 59 countries with the highest maternal and newborn mortality rates would require an additional $1.2bn per year in investments, and would avert an expected additional 87,000 maternal deaths.
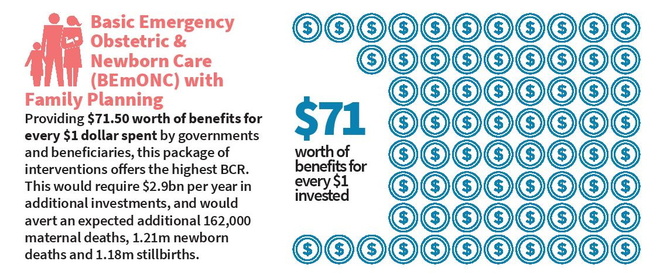
Basic Emergency Obstetric and Newborn Care (BEmONC) in combination with Family Planning
Providing $71.50 worth of benefits for every $1 dollar spent by governments and beneficiaries, the package of interventions with the highest BCR is BEmONC combined with Family Planning. This would require an additional $2.9bn per year in investments, and would lead to an expected additional 162,000 avoided maternal deaths, 1.21m avoided newborn deaths and 1.18m avoided stillbirths.
Among individual interventions, the strongest performing interventions in MNH
The most cost-effective individual interventions when it comes to saving mothers’ lives are the management of eclampsia and pre-eclampsia with magnesium sulfate, which produced the strongest benefit-cost ratios, at 53.0 and 20.7, respectively. This is due to the extremely high fatality rates of these conditions if left untreated and the low cost and high efficacy of the magnesium-sulfate used for their treatment. Removal of retained products of conception left behind in the uterus after childbirth, a condition that if untreated can lead to hemorrhage, sepsis, and death, also presented a remarkably high cost-benefit ratio of 17.1.
When taking into account lifesaving impacts on both mothers and their newborns, the most cost-effective individual intervention was neonatal resuscitation, an intervention requiring only an inexpensive, reusable hand-operated resuscitator, and a health care provider. The second and third most effective interventions were antenatal corticosteroids and assisted vaginal delivery. Similarly, this finding reflects a reduction in asphyxia, and to lesser extent deaths due to prematurity or sepsis, which are among the most common causes of death in the 59 countries analyzed.
* This research was supported by funding from Merck, through Merck for Mothers, the company’s $500 million initiative to help create a world where no woman dies giving life. Merck had no role in the design, collection, analysis, and interpretation of data, in writing of the manuscript, or in the decision to submit the manuscript for publication. The content of this publication is solely the responsibility of the authors and does not represent the official views of Merck.