Ghana Priorities: Rural Sanitation
Technical Report
The Problem
Despite significant government and development partner efforts, Ghana has struggled to improve latrine coverage in rural areas. Since the start of the Millennium Development Goal period in 2000 till the end in 2015, the percentage of rural households practicing open defecation dropped only one percentage point, from 32% to 31%. As of 2017, about 4 million people in rural Ghana practice open defection, while almost 1.5 million have access to improved sanitation.
The burden of diarrhea rates remains high in Ghana. According to the Ghana Health Service 2016 Annual Report, diarrheal disease was the fourth most common disease for all outpatients treated in a health facility. The report also shows that there were almost 800 cases of cholera in Ghana in 2016. The Global Burden of Disease estimates that there were more than 41 million cases of diarrhea and more than 7,000 deaths from diarrheal disease in Ghana in 2017.
Intervention 1: CLTS
Implementation Consideration
The CLTS intervention is structured as a three-step process. First, at the pre-triggering stage, communities are selected for the CLTS intervention, baseline information about the communities is collected, and program implementers are trained. Second, at the triggering stage, the aim is to elicit a sense of shame that will motivate community members to engage with the program and change sanitation behaviors and construct latrines. This is achieved through exercises designed to make people aware of their current unsanitary conditions and practices. In the final step, post-triggering, follow-up visits are conducted to assess the success of the program. In a traditional CLTS intervention, no subsidies are provided.
Costs
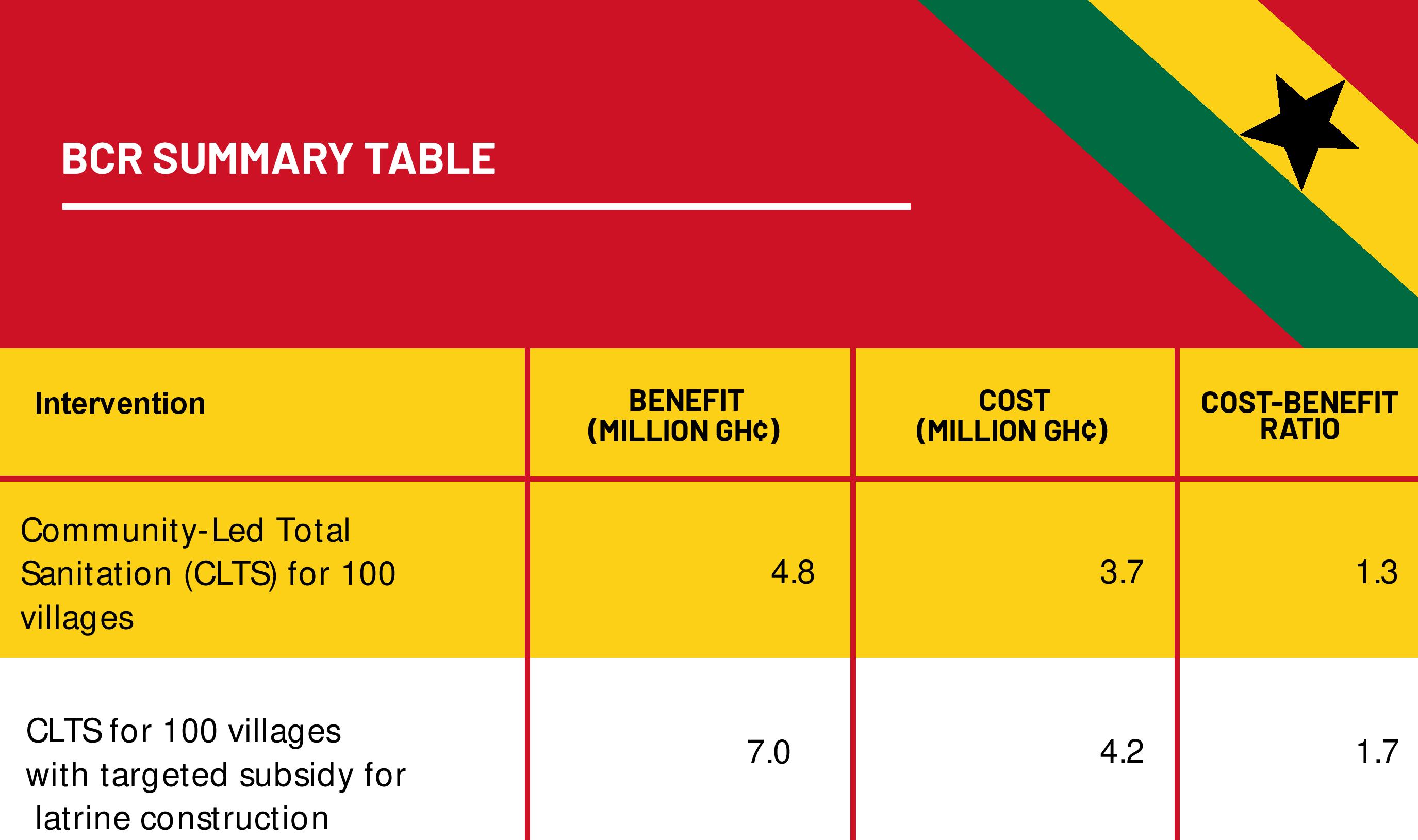
The total costs of this intervention at 8% discount rate are GHS 3,747,915 which include program costs of GHS 1,562,445, time costs of GHS 118,245, capital costs of GHS 1,237,000 and O&M costs of GHS 830,225.
Benefits
Approximately 103, 310, and 721 non-fatal statistical cases of diarrhea are avoided due to this intervention in the low-uptake, medium-uptake, and high-uptake communities respectively. The number of premature deaths averted are about 0.02 per low-uptake community, 0.06 per medium-uptake community, and 0.15 per high-uptake community. The present value of the total benefits of the CLTS intervention is GHS 4,838,700 which includes mortality benefits of GHS 3,815,920, morbidity benefits of GHS 901,715 and time savings of GHS 121,065.
Intervention 2: CLTS + Subsidy
Implementation Consideration
The CLTS plus subsidy intervention would provide 100% subsidies for an improved sanitation technology to all households in the bottom two wealth quintiles in high-uptake communities. These households would be offered vouchers for an improved latrine option whether or not they already have a private latrine. This subsidy is assumed to be provided to the bottom two wealth quintiles based on the finding from the 2016-2017 Ghana Living Standards Survey Round 7 that about 40% of the total rural population fell below the poverty line.
Costs
The total costs of this intervention at 8% discount rate are GHS 4,156,000 which include program costs of GHS 1,562,445, time costs of GHS 118,245, capital costs of GHS 1,463,970, O&M costs of GHS 982,560 and an additional voucher administration cost of GHS 28,780.
Benefits
When a subsidy is coupled with the traditional CLTS intervention, the number of non-fatal cases avoided per high-uptake community increases to almost 1,402 cases. Overall, across the region with 100 communities, covering 15,000 households and 80,500 people, we estimate that the intervention leads to a decrease of 30,910 non-fatal statistical diarrhea cases over the 10-year expected life of the latrine, and a decrease of about 44,542 when subsidies are offered. Further, the number of premature deaths averted in high-uptake villages increases to 0.28 per community. The present value of the total benefits of the CLTS plus subsidy intervention is GHS 6,994,300 which includes mortality benefits of GHS 5,534,945, morbidity benefits of GHS 1,316,075 and time savings of GHS 143,280.